Accelerating burden reduction to elimination
Malaria Consortium is committed to accelerating the reduction in the burden of preventable and treatable diseases such as malaria, pneumonia and dengue, as well as malnutrition and diarrhoea.
Sub-Saharan Africa and southern Asia accounted for over 80 percent of the five million deaths in children under-five in 2020. Children in sub-Saharan Africa have the highest rates of mortality in the world, 14 times higher than the risk for children in Europe and North America. Infectious diseases, including pneumonia and malaria as well as diarrhoea and malnutrition, contribute to a significant number of these deaths in children under five.
These preventable infectious diseases can affect a young child’s mental and physical development, keep older children out of school and adults out of work, contributing to the cycle of poverty and impacting on the prosperity of individuals, communities and whole countries. Such a high burden of disease also puts unnecessary pressure on fragile health systems – accounting for a high percentage of hospital admissions.

Diseases
Our work is focused on the control, management and, where appropriate, the eventual elimination of a range of diseases – malaria, pneumonia, diarrhoea, dengue and neglected tropical diseases. We balance this focus with other factors that affect child and maternal health, including malnutrition.
Learn more
Leading effective interventions
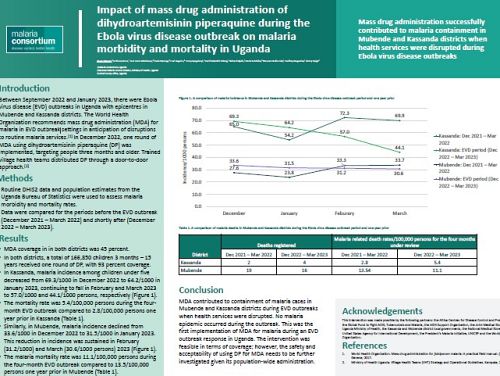
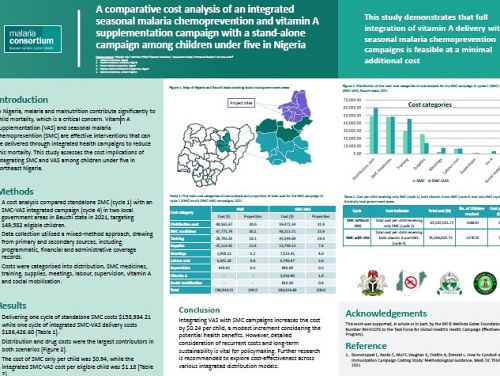
We are a leader in interventions including chemoprevention and vector control, relying on evidence and our expertise to deliver evidence-based interventions.
In practice: We support countries to implement a range of interventions including access and use of long-lasting insecticidal nets (LLINs) and chemoprevention interventions such as intermittent preventive treatment in pregnancy (IPTp) and seasonal malaria chemoprevention (SMC).
Learn more
Building capacity within health systems
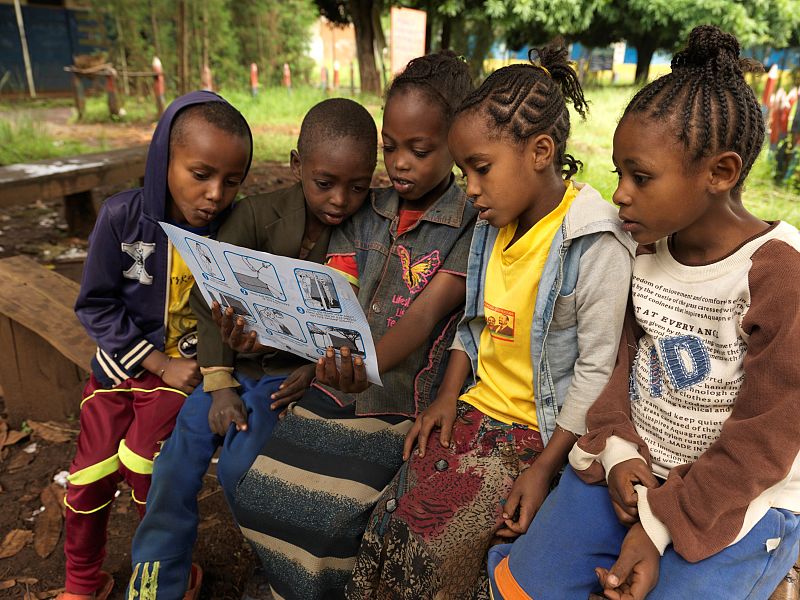
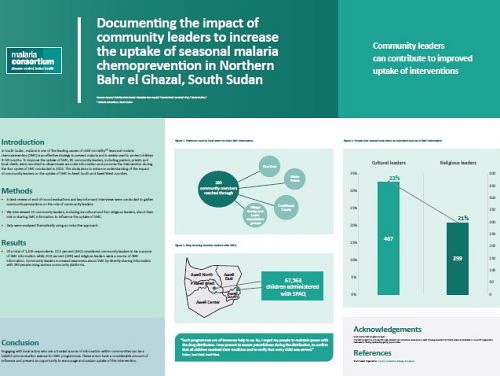
We work with existing community structures, health centres, district health offices and community levels to improve case detection and surveillance in order to build capacity within the community to diagnose and treat diseases quickly and effectively.
In practice: In Ethiopia, community structures such as health extension workers and the health development army play a pivotal role in malaria case detection and surveillance when malaria service provision is disrupted.
Learn more
Implementing community engagement approaches
Since 2003, we have pioneered best practices and have set standards for innovative social and behaviour change (SBC) approaches that promote social accountability; build new approaches to emerging threats; and support the development and introduction of medicines and technologies for disease control. We facilitate communities to engage in dialogues to fill gaps in health information knowledge and support them to develop contextually appropriate solutions to health problems.
In practice: We have implemented the Community Dialogue Approach for neglected tropical diseases and for integrated community case management projects in Mozambique, Uganda, Zambia and Myanmar, linking the intervention into existing health systems and community structures to ensure its sustainability and suitability to the cultural context.
Learn more
Guiding vector control strategies
Limiting the ability of mosquitoes or other insects to spread disease is one of the core strategies to controlling and eliminating malaria and other vector-borne diseases. We work with national government health services and other national and international partners supporting the development of integrated national vector control strategies adapted to various climatic and epidemiological settings and sharing our expertise to manage insecticide resistance. We conduct entomological and epidemiological research to understand impacts of vector control and improve evidence-based selection and deployment of effective interventions.
In practice: In Asia, we act as the implementing agent for the Asia Pacific Malaria Elimination Network (APMEN) Vector Control Working Group, providing capacity to member states, sharing knowledge through online and face-to-face courses, webinars and a web-based information-sharing platform.
Learn more