Antimicrobial resistance (AMR) is a growing threat to our health, causing at least 700,000 deaths globally every year. The death toll attributed to AMR is predicted to rise, with most lives lost in low and middle income countries (LMICs).
AMR is also a critical challenge for many other sectors, including animal health and welfare, aquaculture, agriculture, food safety and broader socioeconomic development. A coordinated, cross-sectoral and multi-pronged approach is needed at all levels of government to ensure an effective and targeted response to this mounting resistance.
No single solution exists to combat the threats associated with AMR. Funders and the pharmaceutical industry must commit to a sea change in research investments for innovations and new technologies to prevent AMR — including diagnostics, vaccines and the search for new antibiotics. Policy makers, particularly in LMICs, must also take ownership by developing and delivering targeted national action plans for AMR, including robust surveillance systems, and introduce rigorous regulation of antimicrobial medicines.
If we fail to curb this growing threat, AMR could cause 10 million deaths annually after 2050 and cost the global economy US$100 trillion (£805 billion) by this date. We must act now before it is too late.
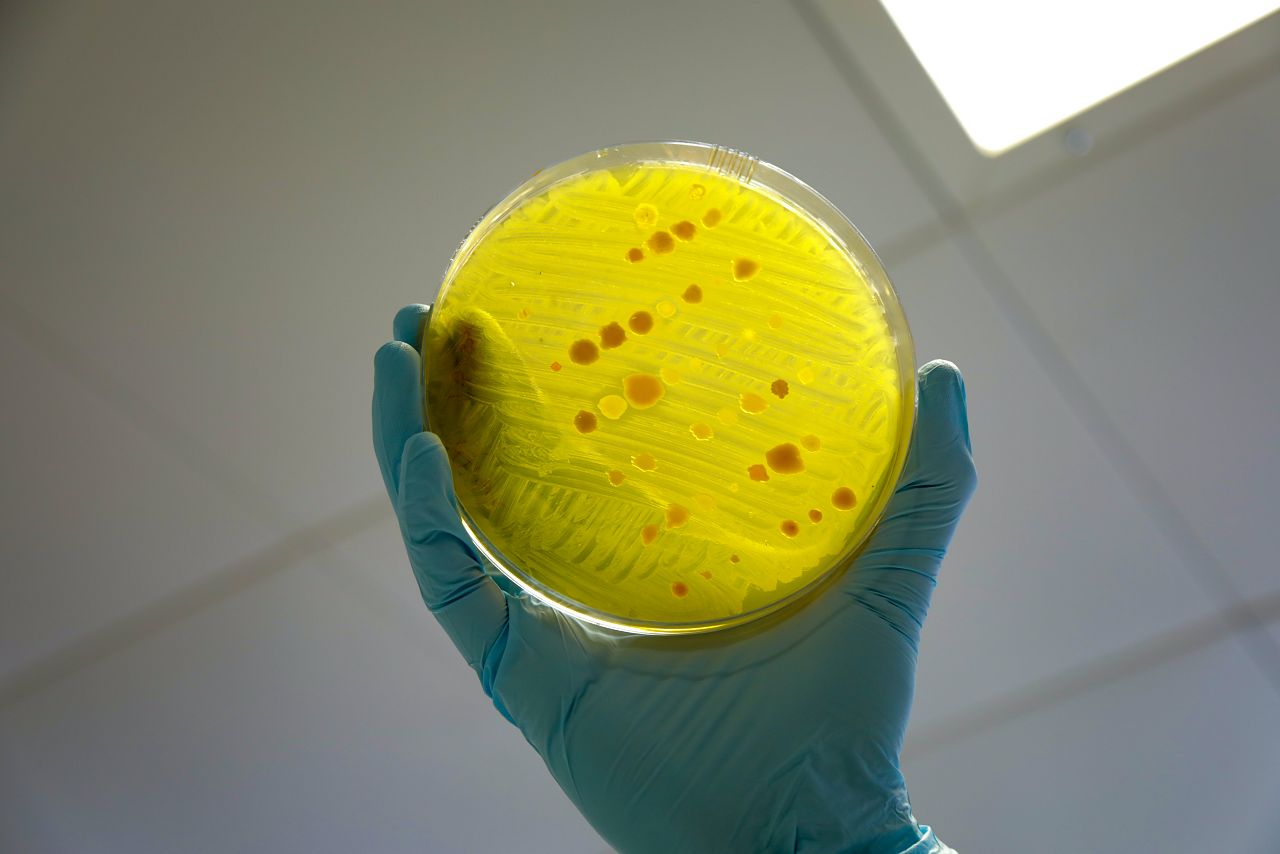
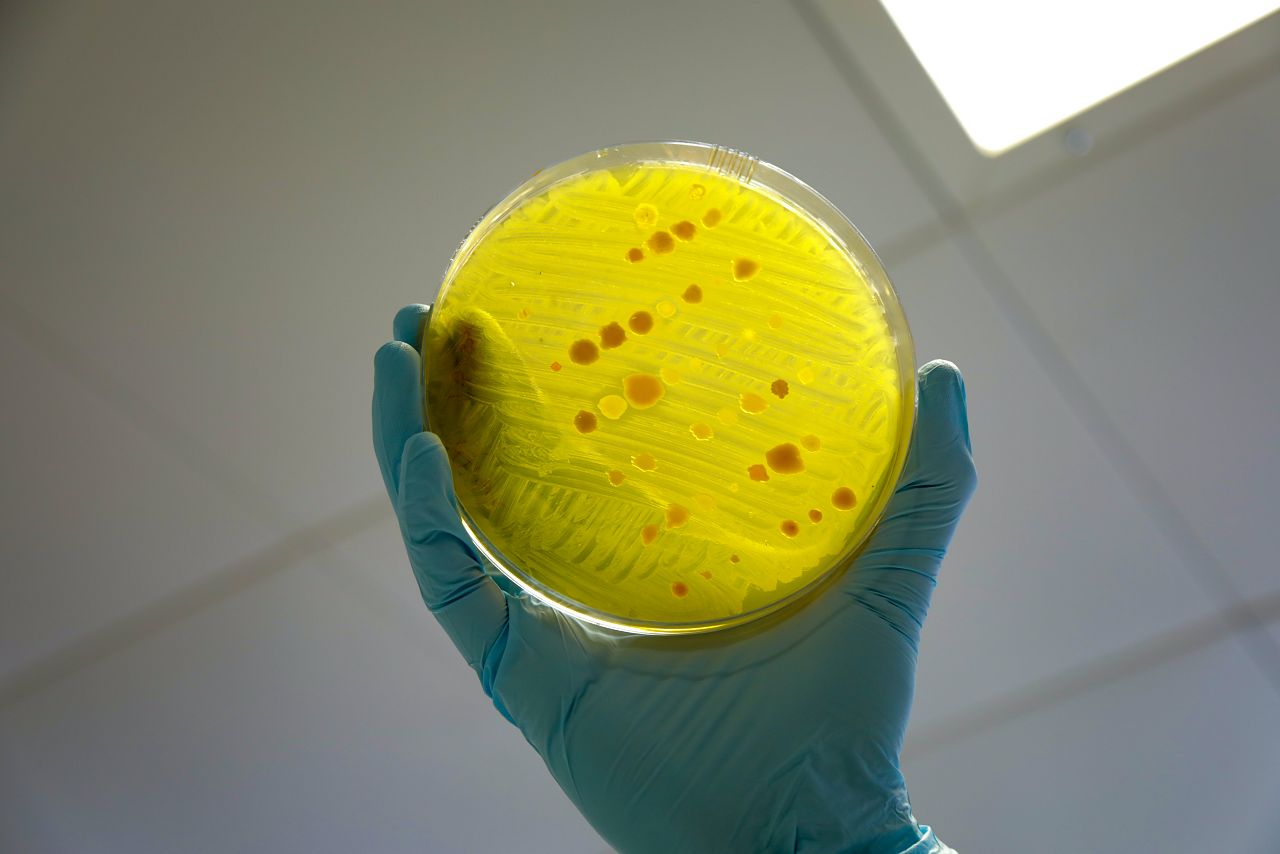
AMR occurs when microorganisms develop the ability to survive the drugs that are designed to kill them. Antimicrobial-resistant drugs are commonly known as ‘superbugs’; examples include drug-resistant gonorrhoea and multi-drug resistant tuberculosis. This resistance arises via natural selection. Some microbes randomly mutate and become able to withstand the effects of medication. As these microbes survive and thrive, drugs become less effective over time and, in some cases, stop working altogether.
AMR, especially in the context of high income countries, is often thought of as synonymous with antibiotic resistance. But the term is used to cover resistance to treatments for infections caused by a wide range of pathogens, including bacteria, parasites, viruses and fungi. AMR, therefore, refers to resistance to bacterial infections (e.g. tuberculosis or bacterial pneumonia), parasitic infections (e.g. malaria), viral infections (e.g. HIV) and fungal infections (e.g. Candida auris).
Although AMR is a naturally occurring phenomenon, the scale and speed with which microbes are developing resistance has accelerated in recent years. There are a number of human and environmental factors causing this.
Driver: Inappropriate or unregulated prescription of drugs
Explanation: Resistance may develop if patients are prescribed drugs for conditions that they cannot treat. For example, antibiotics inappropriately prescribed to treat a viral infection may cause bacteria in a patient’s body to change and become unresponsive to future antibiotics.
Driver: Inappropriate use of drugs
Explanation: Misuse of medicines, such as patients not completing the full course of treatment, means that some microbes may survive and develop resistance to the drug.
Driver: Poor quality and falsified drugs
Explanation: Antimicrobial medicines with insufficient doses of the right ingredients will kill off susceptible strains of microbes but may not be able to destroy more resistant strains. These surviving strains can multiply and contribute to the development of AMR.
When medicines contain different ingredients than those stated, an infection will not be cleared so patients often take another antimicrobial drug. This causes pathogens in the body to be exposed to a different, new drug that should preferably only be used to tackle more resistant infections.
Driver: Intensive use of antimicrobial drugs in animal husbandry, livestock and aquaculture
Explanation: Overuse and misuse of antimicrobials to promote growth and prevent disease in mammals and fish means that microbes are exposed more frequently to the medicines used to treat them and can develop resistance. This may be transmitted to humans via food.
Driver: Environmental contamination
Explanation: Environmental contamination with antimicrobials and resistant microbes occurs through: human and animal waste, pharmaceutical manufacturing waste, and the use of antimicrobials as crop pesticides. Each of these can cause the emergence of resistant microbes in the environment that, once present, have the potential to spread.
Driver: Lack of access to safe water, sanitation and hygiene (WASH)
Explanation: At a community level, the lack of universal access to and use of toilets and safe drinking water, and poor handwashing and food hygiene practices often result in increased infections and diarrhoeal diseases. At healthcare facilities, lack of access to WASH, along with poor infection, prevention and control, is a major driver of healthcare-associated infections, which can become resistant.
Improved WASH at both levels would lead to fewer infections, hence a reduced need for antibiotics and other antimicrobial medicines, and would help to decrease hospital admissions.
AMR threatens to reverse decades of progress across the health and environmental sectors. In particular, the shortage of new drugs is now an urgent problem. Only one major new class of antibiotics has been identified since 1987; the rest have been variations on existing drugs.
This shortage is due to low financial incentives for pharmaceutical drug developers, coupled with long timeframes of the drug development pipeline. With a lack of alternatives currently available, pressure is growing to conserve and protect the antibiotics we do have. Without effective antimicrobials to prevent and treat infections, surgery becomes riskier and prolonged sickness will have a negative impact on human and animal productivity. Treatment costs will also soar. Without urgent action, millions of lives will be at risk, and economies will suffer.
While the global health community and many governments now acknowledge that AMR is a significant challenge affecting multiple sectors, action to date has been insufficient. In 2015, the World Health Organization (WHO) adopted a Global Action Plan on AMR and formed a Tripartite Collaboration with the Food and Agricultural Organization and the World Organization for Animal Health, endorsing a ‘One Health’ approach to combat AMR. The Tripartite Collaboration aims to ensure antimicrobial agents continue to be effective and useful for treating human and animal diseases, promote responsible use of antimicrobials, and ensure good quality medicines are available globally.
Addressing the multifaceted dimensions of AMR is essential if we are to meet the Sustainable Development Goals (SDGs) by 2030. Although not explicitly referenced in the SDG framework, 12 of the 17 goals contain indicators that are AMR-sensitive (i.e. indirectly affected by AMR).
In 2016, United Nations member states came together to agree on multi-sectoral approaches to address resistance. Governments reaffirmed their commitment to develop national strategies and plans to respond to AMR. By 2017, over 85 percent of countries had developed or were in the process of developing national action plans for AMR. National-level measures on infection, prevention and control for human healthcare were in place in 52 percent of LMICs, yet only seven percent had established national surveillance systems for AMR in animals or foods. Those of us working on human health must commit to supporting other sectors at the national level to accelerate progress and close this gap.
Donor governments have also increased action and resourcing to address the problem. For example, the UK government has developed strategies on AMR (2013–2018 and 2019–2024), commissioned an independent review, appointed the first UK Special Envoy for AMR — Professor Dame Sally Davies — and significantly increased funding for AMR through the Ross Fund (a commitment of £1 billion to help combat the world’s most serious diseases). Likewise, in 2017, the European Commission published a European One Health Action Plan against AMR, which aims to position the European Union as a best practice region, influence the global agenda on AMR, and boost AMR research, development and innovation.
However, while many governments have recognised the importance of tackling AMR, more investment is urgently needed to curb resistance.
Partial artemisinin resistance
This refers to 'a delay in the clearance of malaria parasites following treatment with an ACT. As a result, the artemisinin compound is less effective in clearing all parasites within a three-day period among patients who are infected with artemisinin-resistant strains of malaria.
The appropriate use of effective antimalarial drugs is essential for malarial control. Antimalarial drugs can be used as prophylactics for some at-risk populations, such as intermittent preventive therapy for pregnant women or mass drug administration. A nuanced approach, including tailoring and targeting interventions, must be taken to ensure that people who need medicines can access them without worsening the burden of AMR.
Drug resistance is not only a concern for future generations, but is already having serious consequences today. Antimalarial drug resistance has posed a significant challenge to malaria control and elimination. Artemisinin-based combination therapy (ACT) is currently the most effective treatment for tackling uncomplicated Plasmodium falciparum malaria, the parasite species responsible for the most common and deadly form of malaria.
Partial resistance to artemisinin — delayed parasite clearance following treatment — was first reported in P. falciparum at the Thai-Cambodian border in 2008 and has now been confirmed in five countries: Cambodia, Laos, Myanmar, Thailand and Vietnam. While this alone rarely leads to treatment failures in the region, it does mean that it takes longer to clear parasites from the body. Molecular studies have shown that partial artemisinin resistance occurred independently in different places and then spread within the subregion; risk factors associated with its spread include living or working in forests (mainly associated with mobile and migrant workers) and residing in housing without an effective barrier to mosquitoes. At the time of writing, the threat of partial artemisinin resistance has not yet been detected in Africa.
Varying degrees of resistance to partner drug compounds have also been detected. When developing ACTs, drug companies should preferentially use or avoid different partner drugs depending on the resistance profile of local parasite populations to ensure that progress towards achieving elimination is not threatened.
As a leading technical organisation specialising in the prevention, control and treatment of malaria and other communicable diseases, we are gravely concerned about the impact of AMR on public health. While more people in LMICs are currently dying from a lack of access to appropriate treatment than from AMR, this is likely to change unless action is taken to curb drug resistance. AMR has already compromised the efficacy of drugs used to treat some of the common childhood infections we seek to tackle, such as pneumonia and malaria. Unless a One Health approach and strong coordination mechanisms are fully embedded at local, national and global levels, this will only get worse.
We support the objectives set out in the Global Action Plan on AMR:
Our programmatic experience in contexts with antimalarial and antibiotic resistance offers learning for practitioners working on AMR in LMICs. Our approach supports countries to deliver a range of essential activities that directly or indirectly impact AMR.
AMR surveillance is essential if we are to monitor, understand and respond to patterns of resistance, its key drivers and epidemiological trends. Surveillance can help us identify which antimicrobials are not working well and where. However, countries are often at different stages in terms of their capacity for surveillance, including laboratory testing and quality routine data reporting. Robust surveillance systems built upon good quality and timely data can inform decision-making at multiple levels — from health facilities to national governments to international organisations.
A strong surveillance system for antimalarial resistance is in place in relatively low-transmission settings in southeast Asia. We have played a major role in setting up and supporting surveillance and malaria
information systems in Cambodia and Myanmar, as well as conducting national malaria surveys across several countries in the Greater Mekong Subregion. Through our role providing technical assistance to national governments, we have helped to strengthen and align efforts for better reporting, data management and use.
In 2002, routine surveillance activities conducted by Cambodia’s National Malaria Control Programme reported a reduction in efficacy of the antimalarial drug artemether/lumefantrine. This was the first indication of artemisinin resistance in the region, but it took several more years to accrue enough evidence to confirm resistance. While disease-specific surveillance systems — such as for antimalarial resistance — have proved successful, they should align with broader AMR surveillance, where appropriate, for better coordination at national and global levels.
Limited regulation of the quality and distribution of commonly prescribed antimicrobials is a significant concern that contributes to AMR. Strengthened regulation is urgently needed to conserve limited supplies of medicines, particularly of antimalarials.
While substandard and counterfeit drugs remain a major issue for antimalarial medicines, regulatory efforts have so far been comparatively more successful than for antibiotics. For example, in Myanmar oral artemisinin monotherapies — which contribute to drug-resistant malaria — were successfully removed from private sector providers between 2012 and 2014. Similarly, in Cambodia oral artemisinin monotherapies were officially banned by the government in 2009. This led to withdrawal of market authorisation and widespread public dissemination about the ban. Drug inspectors were promoted to the level of Justice Police for the Ministry of Health, and over 400 were trained to conduct regular inspections of drug outlets for artemisinin monotherapies, substandard and counterfeit drugs. As a result, the country saw a decline in unlicensed drug outlets, substandard medicines, and sale and distribution of artemisinin monotherapies.
In addition to increasing regulatory efforts around the availability of medicines, better regulation must also address the challenge of substandard and falsified drugs. Studies have shown that many antimicrobials available in Africa are of ‘questionable pharmacological quality’. Some drugs may also contain very little or none of the active substance of the antimicrobial, or even a different antimicrobial, making them falsified.

Currently, medical diagnosis at the community level is often based on a patient’s symptoms, rather than the use of diagnostic aids. Inaccurate diagnosis means that patients may receive the wrong medicines to treat a disease, or even receive medication they do not require. When coupled with poor adherence to treatment regimes, this presents a very real threat to efforts to curb AMR.
We believe that one promising way to address this is by supporting community health workers (CHWs) — volunteers who provide basic healthcare services in their often remote communities — to accurately test, diagnose and treat malaria, pneumonia and diarrhoea in children under five. Known as integrated community case management (iCCM), this approach sees CHWs trained on different diagnostic aids (e.g. malaria rapid diagnostic tests (mRDTs) and respiratory rate monitors), equipped with treatments including ACTs, antibiotics, oral rehydration salts and zinc, and regularly supervised. We know this approach works when implemented well, and believe it would be an effective way to reduce the incorrect prescription of antimalarials and antibiotics that often takes place in the informal private sector.

It is widely acknowledged that education alone will not change behaviour; however, it can be a prerequisite. In the case of AMR, increased consciousness of and education around the causes of resistance and ways to address it are still needed. Indeed, the 2016 Review on AMR recommended a massive global awareness campaign that would target global, regional and national levels.
Social and behaviour change (SBC) at the community level is also essential for raising awareness of AMR, shaping related social norms and, ultimately, changing behaviour. Interventions must reflect that there are both supply and demand factors in play. To address the former, we must seek to understand what motivates informal private drug suppliers to sell antimicrobials over the counter without a prescription — as well as what would encourage them to cease this practice — and design interventions accordingly. Similarly, to address the latter we must identify what drives communities’ demand for antimicrobials, and devise SBC activities that encourage them to only take these when prescribed by a trained medical professional or health worker and to adhere to prescription guidelines.
Applying SBC interventions across the human health, agricultural and animal sectors, as part of a One Health approach, should increase communities’ understanding of the drivers of AMR and encourage them to play a significant role in developing and adopting sustainable solutions. For example, SBC could promote handwashing to prevent the spread of disease, encourage the hygienic preparation of foods and dissuade farmers from using antibiotics for disease prevention or growth of healthy livestock — thereby playing a key role in infection prevention control.
The development of diagnostic aids, vaccines and treatments can contribute to reducing the need for and lessen the pressure on existing antimicrobials. For example, the development and rollout of a simple, point-of-care mRDT — that uses a finger-prick of blood to determine whether an individual has malaria — can help to ensure that only those who test positive are given antimalarials, thereby avoiding the overconsumption or misuse of such drugs. mRDTs are particularly useful in rural areas and/or where health workers cannot easily access good quality microscopy services. Systems must be in place in malaria-endemic countries to ensure that mRDTs are used correctly by health workers and are affordable.
Vaccines also play an important role in tackling AMR. By preventing deadly diseases, they contribute to conserving the existing supply of antimicrobial medicines whose efficacy may already be in decline. We welcome ongoing efforts to develop an effective malaria vaccine — an important tool for malaria control and elimination. The RTS,S/AS01 vaccine — which is being piloted through national immunisation programmes in parts of Kenya, Ghana and Malawi (2019–2022) — has previously been found to provide partial protection against malaria in young children, preventing approximately four in 10 cases.
In addition to improved diagnostic aids and vaccines to help prevent the spread of AMR, funders and industry must increase investment in finding new drugs to treat drug-resistant infections, as well as a new class of antibiotics. Public, private and philanthropic partnerships should pursue such initiatives to address this pressing global health threat.
Our work has contributed to the prevention and management of AMR, but much more remains to be done. To make strides towards tackling this issue globally and within LMICs, we propose the following:
Tackling AMR is a race against time. Without immediate action, AMR will make it considerably more difficult to achieve universal health coverage. As such, governments must ensure the most remote and marginalised communities have access to accurate diagnosis and quality treatment through trained health workers, as opposed to via the informal private sector. Investing in CHWs through community-based primary healthcare programmes such as iCCM will simultaneously prevent AMR and achieve health coverage for all. Ensuring that national AMR action plans are developed and implemented will be crucial to this endeavour.
Donors play a key role in addressing the global burden of AMR, and can support LMIC governments to increase domestic spending on the issue. Their investments should support countries to monitor the current AMR burden and seek to build local capacity to make expedient decisions based on timely and reliable surveillance data. National surveillance efforts should also be aligned with WHO’s Global Antimicrobial Resistance Surveillance System to ensure efficient integration; greater coherence should increase the likelihood that trends are spotted and acted upon early.
Governments should consider stronger regulation of antimicrobial medicines to ensure these are only available by prescription from a trained health professional. Governments who have begun to develop such regulatory environments should share their learnings with others who are looking to develop their own processes. For regulation to be effectively implemented, communities must be informed and engaged in the process and careful monitoring must be conducted.
While CHW programmes are tailored according to country contexts, iCCM should be integrated into community-based primary healthcare programmes to enable CHWs to diagnose and treat common childhood diseases accurately, thereby contributing to the reduction of the burden of AMR by avoiding misuse of antimicrobials. Experts working in this field can provide guidance and best practices around regular supervision and training to ensure high levels of adherence to guidelines.
While many donors recognise that tackling AMR will require a holistic approach, there have been relatively few funding calls for related SBC approaches. Yet SBC should be seen as an intervention in itself. More research is needed to identify what drives behaviour and how collective action approaches like community dialogues can be scaled up and sustained.
Strengthening diagnostic tools is essential to alleviating the overconsumption of antimicrobial medicines. In many LMICs, diagnosis is currently insufficient at the community level, so improving diagnostic algorithms, access and affordability should be prioritised. Field testing of any new devices must take place to ensure adherence both to the device requirements and to case management protocols.