We have curated a list of Malaria Consortium publications for ASTMH 2021.
Browse through the publications below to find out more about some of the topics that the Malaria Consortium team will be talking about, including our work and research on COVID-19 and malaria, intermittent preventive treatment in infants (IPTi ) and seasonal malaria chemoprevention.
COVID-19
-

Evaluating the impact of COVID-19 on malaria and other infectious diseases in Uganda: Understanding comorbidities
Countries in sub-Saharan Africa carry a disproportionately higher share of the global burden of malaria and other infectious diseases. The potential impact of COVID-19 on the diagnosis, prevention and treatment of endemic diseases is, therefore, of critical concern. Uganda is an ideal setting in which to investigate this impact, given the country’s high burden of malaria and numerous cases of COVID-19 to date. This project seeks to understand the burden chiefly of malaria (but also of TB and HIV/AIDS) among patients with COVID-19, and to assess the clinical consequences of potential interactions. -
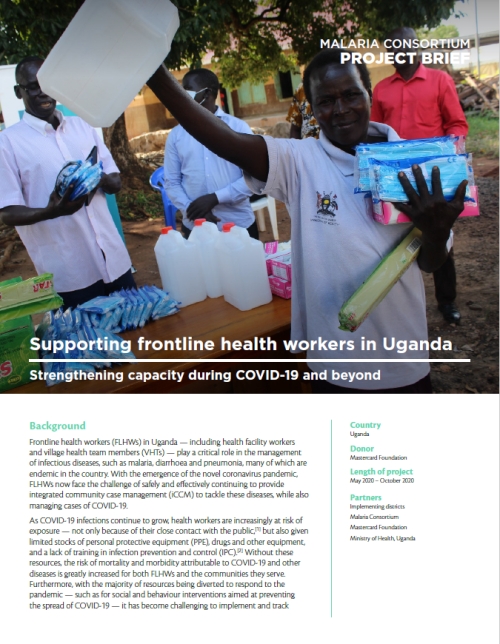
Supporting frontline health workers in Uganda: Strengthening capacity during COVID-19 and beyond
Frontline health workers (FLHWs) in Uganda play a critical role in managing infectious diseases, many of which are endemic in the country. The COVID-19 outbreak has made this work even more challenging. This project, in partnership with Mastercard Foundation, aims to develop the capacity of FLHWs to diagnose and treat cases of COVID-19 while continuing to provide community case management services safely, accurately and with the right tools and support.
Seasonal malaria chemoprevention
-
Exploring the implementation of seasonal malaria chemoprevention in Mozambique
In 2020, the Mozambican National Malaria Control Programme and Malaria Consortium initiated a phased implementation project in Nampula province to assess the feasibility and effectiveness of seasonal malaria chemoprevention (SMC) in the Mozambican context. Between November 2020 and February 2021, we delivered SMC to a target population of around 72,000 children under five in the districts of Malema and Mecubúri. We also conducted an end-of-round coverage survey in these districts, coordinated by Centro de Investigação em Saúde de Manhiça, after the final cycle of the annual SMC round. -
Co-implementing vitamin A supplementation with seasonal malaria chemoprevention: A pilot implementation study in Sokoto state, Nigeria
In 2019, we conducted a pilot implementation study in Sokoto state, Nigeria to to assess the feasibility and acceptability of integrating vitamin A supplementation with the seasonal malaria chemoprevention programme. This research brief details the study's innovative findings and provides pragmatic evidence that could guide implementation and scale-up, as well as recommendations for donors, implementers, national and state malaria programmes, and researchers. -
Evaluating the feasibility, acceptability and protective effectiveness of seasonal malaria chemoprevention in Karamoja, Uganda
Malaria Consortium is supporting Uganda’s National Malaria Control Division to conduct a hybrid effectiveness and implementation research study in three districts of Karamoja, northeast Uganda. The feasibility, acceptability and impact of seasonal malaria chemoprevention in areas with high resistance is unknown. With our study, we aim to address this knowledge gap. -
Using the role model approach to improve administration of seasonal malaria chemoprevention drugs in Burkina Faso, Chad and Togo
Seasonal malaria chemoprevention is delivered in monthly cycles during the malaria season using two antimalarial drugs: sulfadoxine-pyrimethamine (SP) and amodiaquine (AQ), or ‘SPAQ’. The role model approach is a community-driven behaviour change strategy that identifies existing strengths or solutions among individuals in a community, which are then shared with other community members to bring about positive changes in behaviour. We explored this approach to address the challenges associated with SPAQ administration in Burkina Faso, Chad and Togo, and to find existing, local solutions for improvement.
IPTi
-

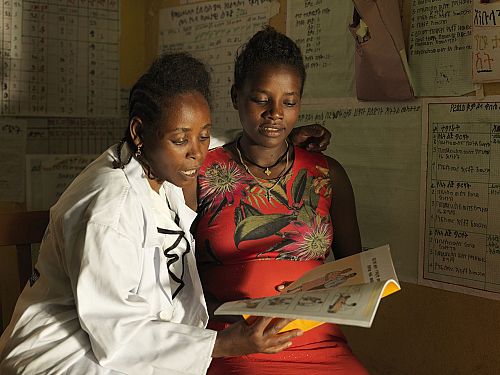
Reducing malaria morbidity in infants through intermittent preventive treatment in Nigeria
To reduce malaria morbidity and mortality in infants, the World Health Organization (WHO) recommends intermittent preventive treatment in infants (IPTi) with sulfadoxine-pyrimethamine in areas with moderate to high malaria transmission. However, a decade after WHO’s recommendation, only one country has adopted the strategy as national policy, and various barriers to IPTi policy uptake remain. This study will assess IPTi’s clinical effectiveness and operational feasibility in Nigeria. It aims to generate the necessary evidence to support the intervention’s uptake in the national health policy.
Surveillance, malaria control and neglected tropical diseases.
-
Facilitating evidence-informed programming in Mozambique
This learning paper shares key lessons learnt from developing and deploying an integrated malaria information storage system at the district and health facility levels in Mozambique. It gives recommendations on how to set up a functional and responsive malaria surveillance system. Despite disruptions caused by COVID-19, the project met several key milestones, including testing the system and successfully rolling out a complex training scheme. -
Supporting government to control malaria in Uganda
USAID’s Malaria Action Program for Districts aims to reduce malaria-related childhood and maternal morbidity and mortality in Uganda. The project provides technical and programmatic support to central and local governments to increase the impact and reach of malaria prevention and diagnostic services. It also aims to strengthen the government’s capacity to design, plan and monitor malaria control activities -
Improving neglected tropical disease (NTD) services and integrating into primary healthcare
Neglected tropical diseases (NTDs) continue to affect more than one billion people worldwide, disproportionately impacting the most vulnerable and marginalised communities. With one of the highest NTD burdens in Africa, Ethiopia is implementing a new project that will explore the feasibility, acceptability and cost effectiveness of integrating the prevention, diagnosis, management and reporting interventions of three common NTDs into Ethiopia’s primary healthcare system. -
Prevention, diagnosis and management of podoconiosis: Developing resilient health systems in Ethiopia
Podoconiosis is a non-infectious neglected tropical disease (NTD) caused by exposure to volcanic soils. It disproportionally affects poor and marginalised communities. Globally, around four million people are estimated to suffer from podoconiosis — over a third of those affected live in Ethiopia. This research project aims to improve prevention, diagnosis and management of podoconiosis in Ethiopia’s primary healthcare system.