Mozambique
Malaria is highly endemic in Mozambique, accounting for four percent of malaria cases globally. The entire country is at risk, with the highest prevalence of the disease in the north and along the coast. Nearly half of the population lives below the poverty line and those in rural communities lack access to basic healthcare services contributing to excess morbidity and mortality. We work alongside the Ministry of health and National Malaria Control Programme to strengthen the country’s health system and reduce the malaria burden.
Malaria Consortium in Mozambique
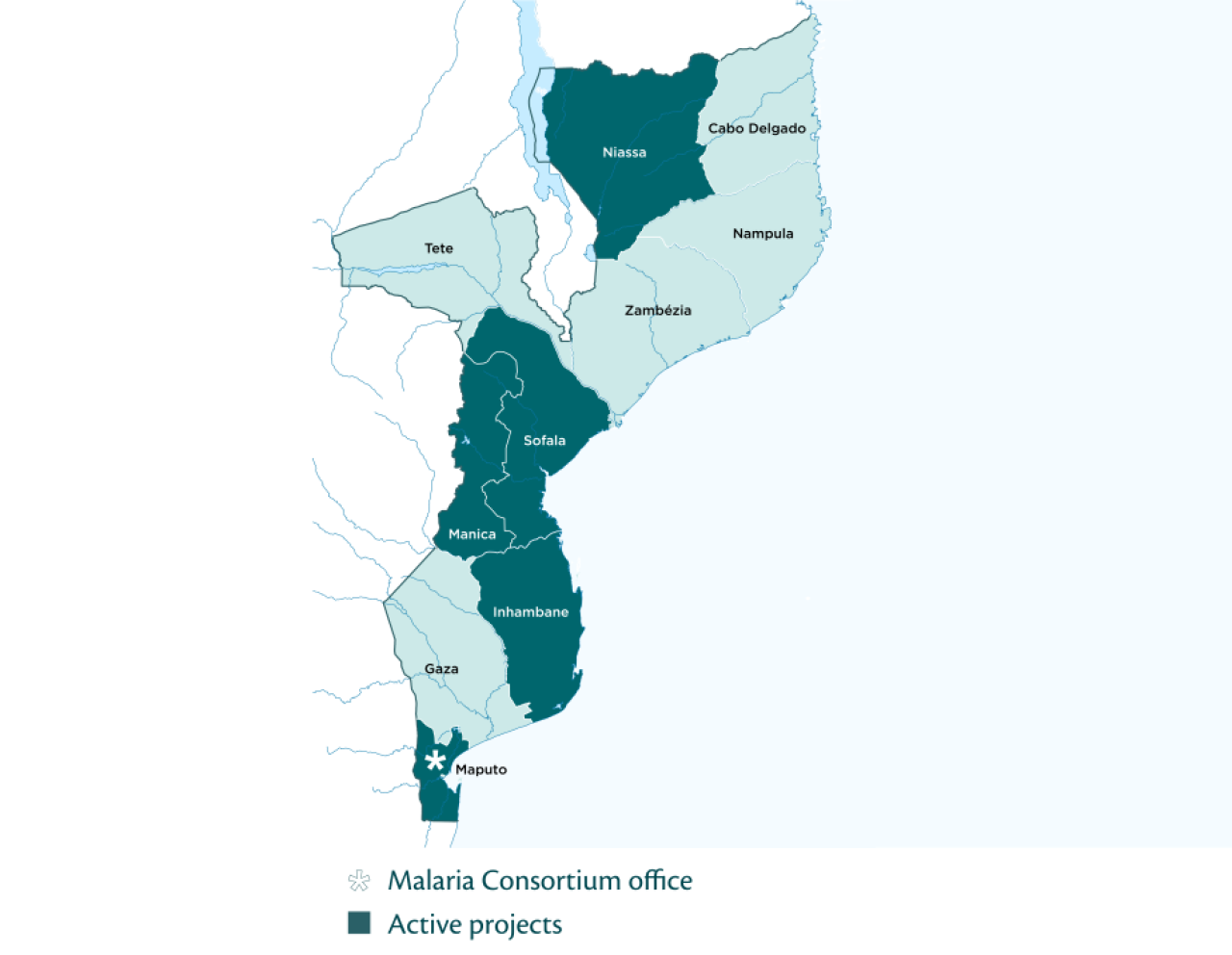
Malaria Consortium has been working in Mozambique since 2005 with an office in Maputo, Mozambique’s capital, and are committed to reducing the burden of malaria and other communicable diseases in Mozambique, with particular focus on those affecting children under five. We work closely with the Ministry of Health (MoH), the National Malaria Control Programme (NMCP), the National Community Health Workers Programme, provincial and district health authorities and affected communities.
We provide technical assistance to our partners to strengthen existing health systems by improving the integrated community case management (iCCM) of common illnesses, such as malaria, diarrhoea and pneumonia; deploying functional surveillance mechanisms; developing and scaling innovative community-focused platforms to facilitate data informed decision-making; filling knowledge gaps through operational research; and organising social and behaviour change activities.