Neglected tropical diseases
Neglected tropical diseases (NTDs) – a group of parasitic and bacterial infections mostly concentrated in sub-Saharan Africa – affect over 1.7 billion people worldwide, causing chronic disability, stigma, ill health and half a million deaths each year. These diseases disproportionately affect the most vulnerable.
Malaria Consortium has worked on NTD control since 2005, aiming to ensure access to effective prevention and treatment by supporting the integration of NTD control into health systems. We conduct situational analyses, review possible interventions and develop new responses to NTD challenges across Africa and Asia. We also promote a holistic approach that emphasises the engagement of the education sector, community and primary healthcare structures.
We are an active member of the UK Coalition Against NTDs, supporting efforts to foster communication and information-sharing between agencies invested in the long-term, sustainable control and elimination of NTDs. This collective approach is vital in ensuring that NTD control is included within health development frameworks.

Our publications
Our NTD-related publications include journal articles from our cutting-edge operational and implementation research, project briefs, case studies, learning briefs, presentations and capacity statements about universal health coverage (UHC) and our work with communities and governments from several countries affected by NTDs including Bangladesh, Cambodia, Myanmar, Nepal, Thailand, South Sudan and Ethiopia.
Learn more
Integrating NTD approaches into primary healthcare systems
Primary healthcare systems and community structures are crucial in effective case management, from case detection in the early stages, to home care management for disability, to delivering essential treatment for NTDs.
In practice: Our NTD intervention in Ethiopia improved the primary healthcare system’s capacity to detect, manage and record three common NTDs in the country.
Learn more
Community dialogues for NTD prevention and control
The prevention and control of NTDs requires a strategic, community-based approach to behaviour change.
In practice: In Mozambique, we used the community dialogue approach to establish the sense of community ownership and social accountability that is essential for securing sustained social and behaviour change to improve health outcomes.
Learn more
Improving NTD control and surveillance
We assist governments in the development of tools to facilitate the primary health care system in understanding disease trends and using data for disease control and surveillance.
In practice: In Myanmar, we supported the roll-out of revised dengue prevention and control guidelines.
Learn more
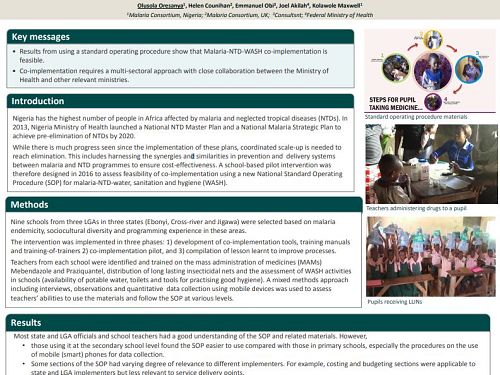
Mass drug administration
We use our experience in the mass distribution of long-lasting insecticidal nets (LLINs) and seasonal malaria chemoprevention (SMC) to improve mass drug administration (MDA) for NTDs.
In practice: In Nigeria, we co-implemented malaria, NTD and water, sanitation and hygiene interventions in schools.
Learn more
Vector control
We integrate vector control activities for insect vector-borne diseases including dengue into our core areas of work, researching the impact of the most effective intervention to prevent disease.
In practice: In Cambodia, we implemented a cross-sectoral dengue prevention project to contribute to the development of knowledge around effective dengue control strategies within communities.
Learn more