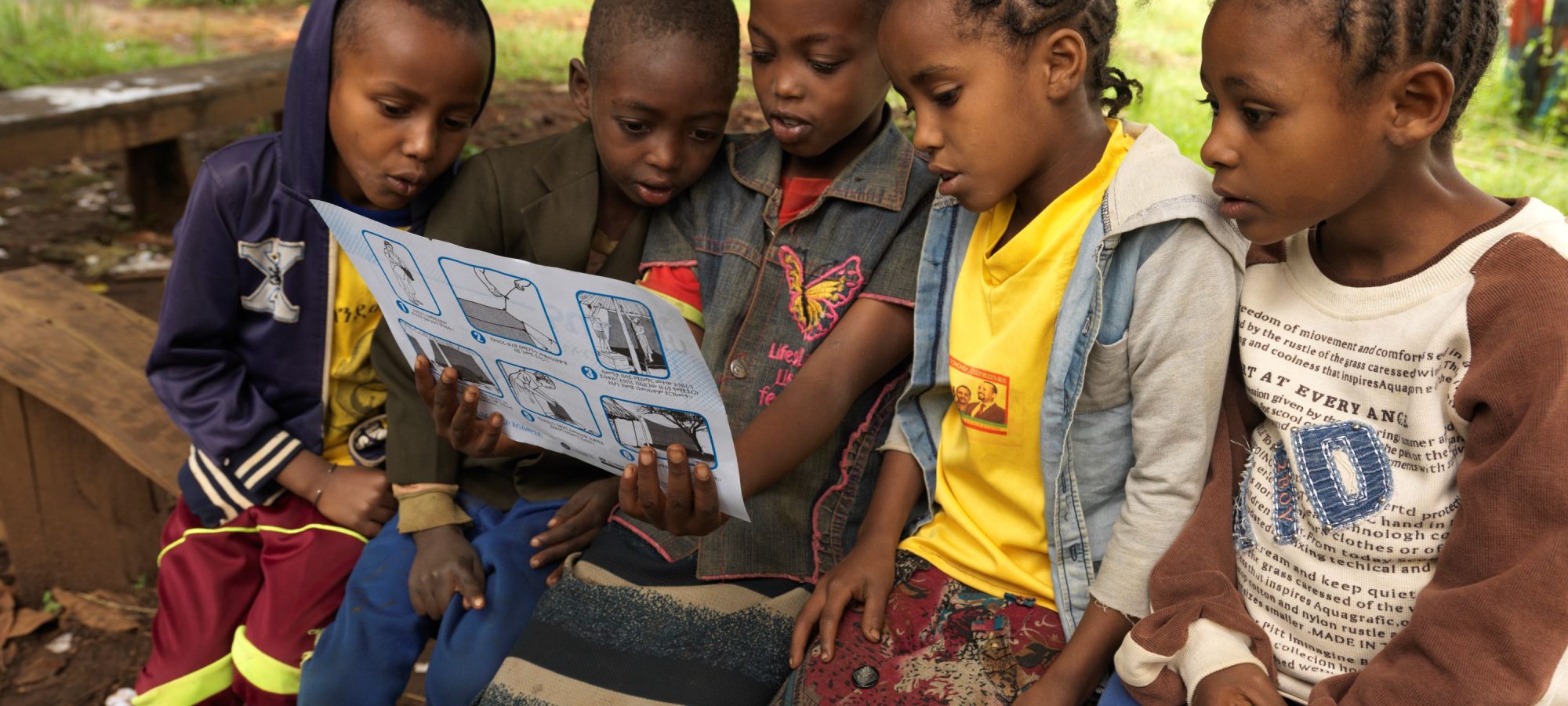
World Malaria Day 2024: Young people engaged through antimalaria school clubs as agents of change in malaria control
Despite being preventable and treatable, malaria threatens the lives of 3.2 billion people around the world. Every year, the disea......read more