Global health security
With globalisation comes opportunity and prosperity. However, a consequence of an inter-connected world that is constantly on the move is the potential threat of disease outbreaks spreading faster, more widely and more erratically than ever before.
It is not uncommon for infectious diseases originating in Africa or Asia to be found in Europe or the US, for example, soon after a particular outbreak. Some of the more well-known and recent pandemics include Ebola, yellow fever, cholera (in Africa); avian flu (in Asia); Middle East Respiratory Syndrome (MERS-CoV); and Zika (in the Americas).
In addition to the potential of rapidly spreading infectious pathogens across the globe, the growing spread of antimicrobial drug resistance (AMR) is another concern for global health security. AMR is the ability of bacteria, viruses and some parasites to stop drugs such as antibiotics or antimalarials from working. As a result, life-saving treatments are no longer effective leading to the spread of diseases which are resistant to available treatments. Contributing to the rise of AMR is inadequate diagnosis and treatment practices among health workers despite national guidelines, poor patient adherence to treatment, and the availability of counterfeit and substandard drugs.
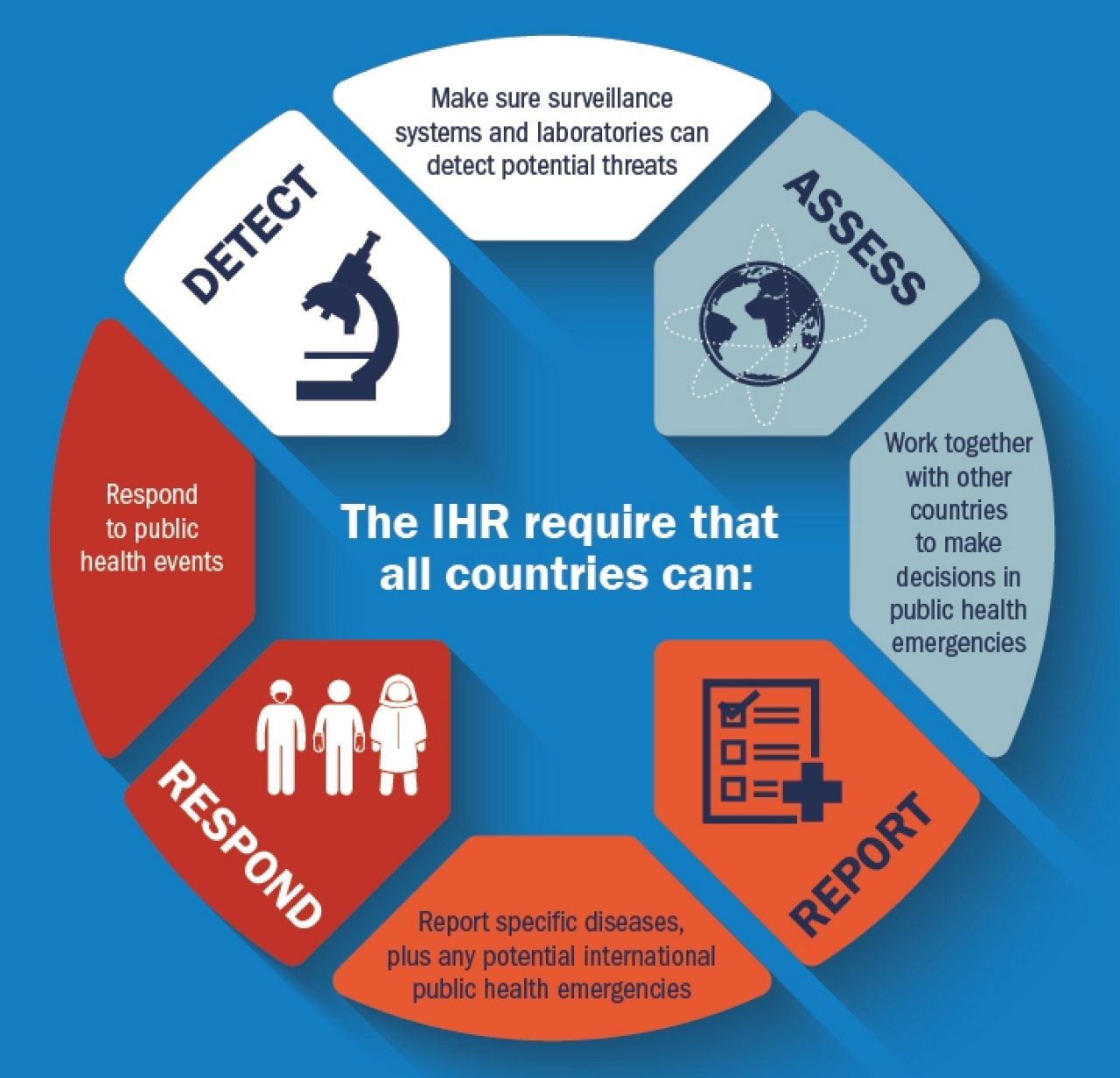
Biological threats and the spread of drug-resistant infectious diseases, such as resistant strains of the malaria parasite, present a growing danger to global health security. These emerging global pandemic threats required a global solution and this led to the development of the legally binding International Health Regulations (IHR). These were approved by all 194 member states of the World Health Organization (WHO) who agreed to work together to support global health security and to report events of international public health importance. It is the responsibility of the WHO to support signatories to the IHR to comply with the rules. It is thanks to these regulations that we now have a strong global response to any threats that might arise.
Source: Centers for Disease Control and Prevention
Global Health Security Agenda

Source: No More Epidemics
The Global Health Security Agenda (GHSA) was launched in 2014 and provides a structure to help countries reach IHR compliance. It aims to help build countries’ capacity to help create a world safe and secure from infectious disease threats and to elevate global health security to be a national and global priority.
The GHSA is a multilateral and multi-sectoral approach to strengthen both global and nations’ capacity to prevent, detect and respond to human and animal infectious disease threats. Critical elements to this security include strong health systems and robust surveillance, detection and response mechanisms. The GHSA Joint External Evaluation tool is offered to countries to assist them to identify the most urgent needs within their health security system and to find and prioritise opportunities for improved preparedness, response and action.
What is Malaria Consortium doing?
Prevent
- Vector control: We are implementing large-scale vector control programmes for malaria prevention in several countries, and aim to provide innovative vector control projects to help prevent mosquito-borne disease outbreaks for diseases such as dengue, Zika and chikungunya. We are also strengthening efforts to control the movement of drug resistant malaria parasites through our cross-border malaria project in Cambodia, which catches and treats mobile workers who may be carrying resistant malaria parasites. We are also conducting Aedes insecticide resistance studies in the country. The evidence from our work is helping to inform policy development.
Detect and Respond
- Strengthening surveillance systems: We provide technical support to national health systems to build their capacity to detect and respond to disease outbreaks and to understand patterns of antimicrobial and insecticide resistance. We do this by training surveillance staff at all levels, and by researching novel approaches to help identify resistant strains of malaria parasites. In Uganda, for example, we have provided entomological surveillance to observe changes in transmission and supported the National Malaria Control Programme to develop comprehensive malaria epidemic response plan. We also supported Kibale District during the Ebola outbreak with in health education and trained health workers in infection prevention, supporting the setup of waste pits and incinerators.
- Antimicrobial resistance: We are currently engaged in a study that explores the use of community dialogues, a community engagement approach pioneered by Malaria Consortium and used across a range of different contexts, for preventing and controlling antibiotic resistance in Bangladesh. We also contribute to reducing antimicrobial resistance through the development of quality controlled supply chains and improved stewardship, for example through our seasonal malaria chemoprevention
- Bio-surveillance: We are training lab workers, local government leaders and/or emergency health workers to strengthen their capacity to engage in bio-surveillance and detect new outbreaks of disease, either malaria or other non malaria fevers.
- Improving diagnosis and treatment of febrile illnesses: In order to mitigate the spread of antimicrobial resistance we believe it is extremely important that innovative tools for differential diagnosis of febrile illness continue to be tested and that health providers are trained on how to identify the causes of fever accurately. Knowing when it is appropriate to use antibiotics to treat bacterial infections reduces the likelihood of the wrong drugs being given and therefore preventing the development and spread of antibiotic drug resistance.
To support these efforts, we are testing pneumonia diagnostics in various countries, and we are strengthening community-based diagnosis and treatment of malaria, pneumonia and diarrhoea in rural areas.
We also work with government drug administration agencies to ensure health workers and drug shop owners limit the inappropriate use of antimalarial drugs and only dispense treatments of pre-qualified drugs to those who have tested positive to malaria.