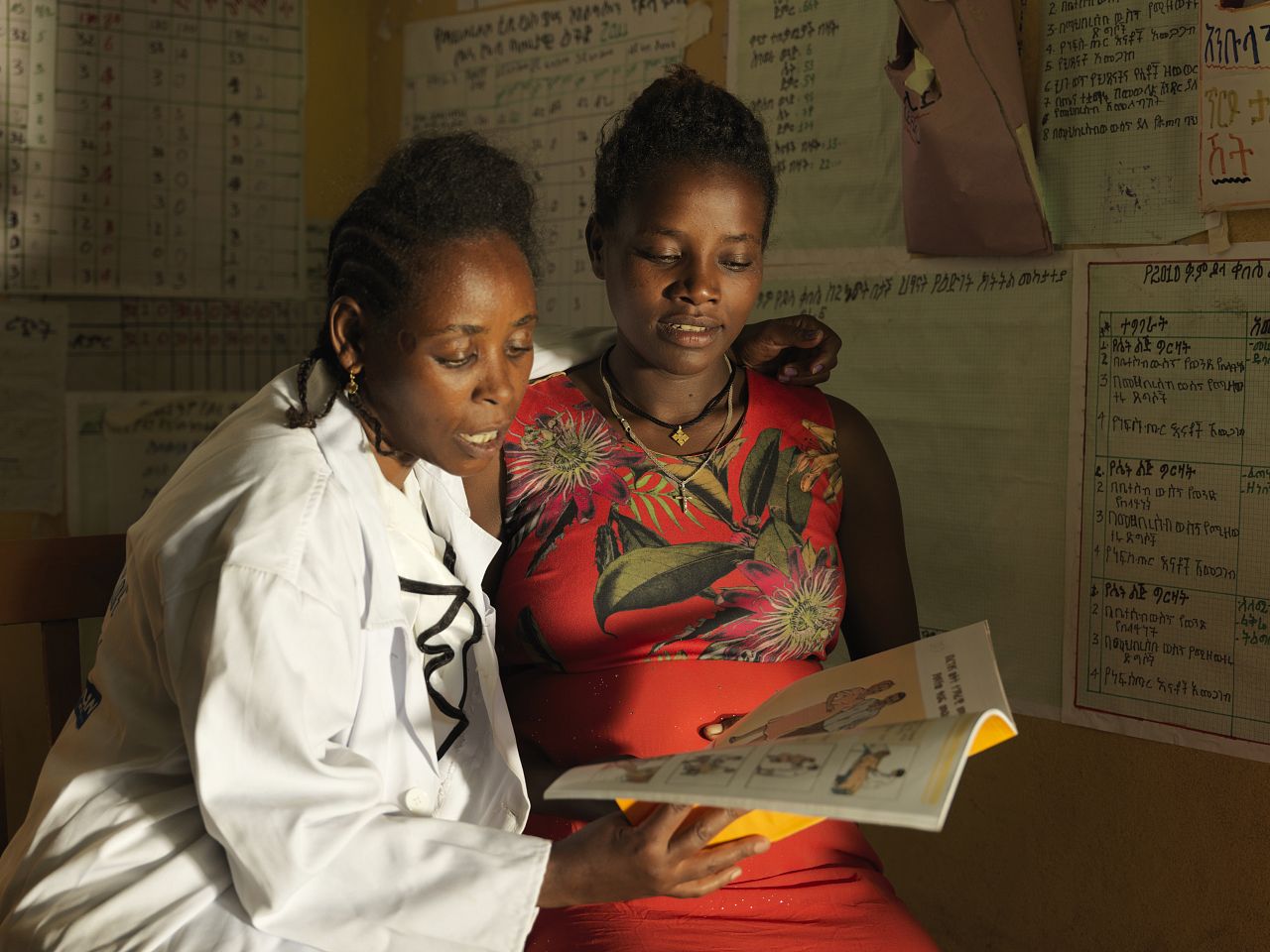
Case management
We seek to improve the management of cases of disease and illness through community-based healthcare delivery. We work closely with public and private health structures to improve accurate diagnosis of diseases and strengthen referral systems from community to facility level for priority cases. We also train local health workers to strengthen case management processes and ensure correct, quality-assured treatments are given.
Integrated community case management
The integrated community case management (iCCM) approach involves providing capacity development training and building support for community health workers (CHWs) to readily recognise, diagnose, treat and refer, where indicated, cases of common childhood illnesses and disease. These CHWs are people within the community and include those with limited education and medical training.
In practice: In Uganda, we worked with the Ministry of Health to strengthen referral systems for under-fives with danger signs and expand iCCM for maternal and child survival.
Learn more
Delivering health services in hard-to-reach areas through community-based primary healthcare
Community-based primary healthcare (CBPHC) involves using community-level health workers to deliver health services to under-served communities in remote areas.
In practice: In Myanmar, we provided further training to existing malaria volunteers – already trained by the NMCP to diagnose and treat malaria in their communities – to diagnose and treat pneumonia and diarrhoea and detect malnutrition in children under five.
Learn more
Using digital tools to improve the quality of care
Digital tools can guide community-level health workers through patient registration, assist with diagnosis, advise on treatment and referrals, and allow supervisors to monitor performance and improve resource allocation.
In practice: Through upSCALE – a mobile health system strengthening project in Mozambique – we strengthened linkages between communities and formal health facilities to improve the quality of community-based health interventions.
Learn more
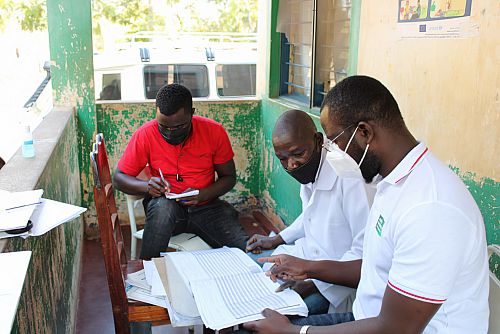
Improving disease surveillance through existing community structures
Community-level health workers play a pivotal role in malaria case detection and surveillance and are the first point of healthcare provision to communities.
In practice: In Ethiopia, we worked with existing community structures, health centres, district health offices and community levels to improve malaria case detection and surveillance.
Learn more
Promoting preventive behaviours through community dialogues
Social behaviour change communication activities such as community dialogues are used to encourage the use of services, increase levels of health knowledge and community service delivery acceptance, and work with communities to develop community led solutions to problems identified, encouraging self-reliance and resilience.
In practice: Contributing to efforts to tackle antimicrobial resistance in Bangladesh and Nepal, we’re working with project partners to implement and evaluate a community engagement intervention.
Learn more
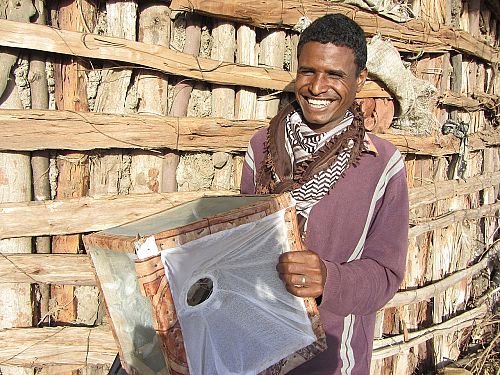
Improving the delivery and uptake of drugs
We also work with communities to improve delivery and uptake of highly effective and affordable drugs, such as for seasonal malaria chemoprevention and mass drug administration for neglected tropical diseases.
In practice: Through our seasonal malaria chemoprevention programme in countries across the Sahel, we work with national governments to provide technical, logistical and financial support to SMC campaigns to ensure as many children aged 3-59 months benefit from the highly effective intervention.
Learn more