Our pneumonia diagnostics team held a number of interesting sessions at the American Society of Tropical Medicine and Hygiene (ASTMH) in Philadelphia from 25-29 October, 2015. These sessions covered findings, challenges and lessons learnt over the past two years from our work on finding the best tools for diagnosing pneumonia – a major childhood killer in sub-Saharan Africa.
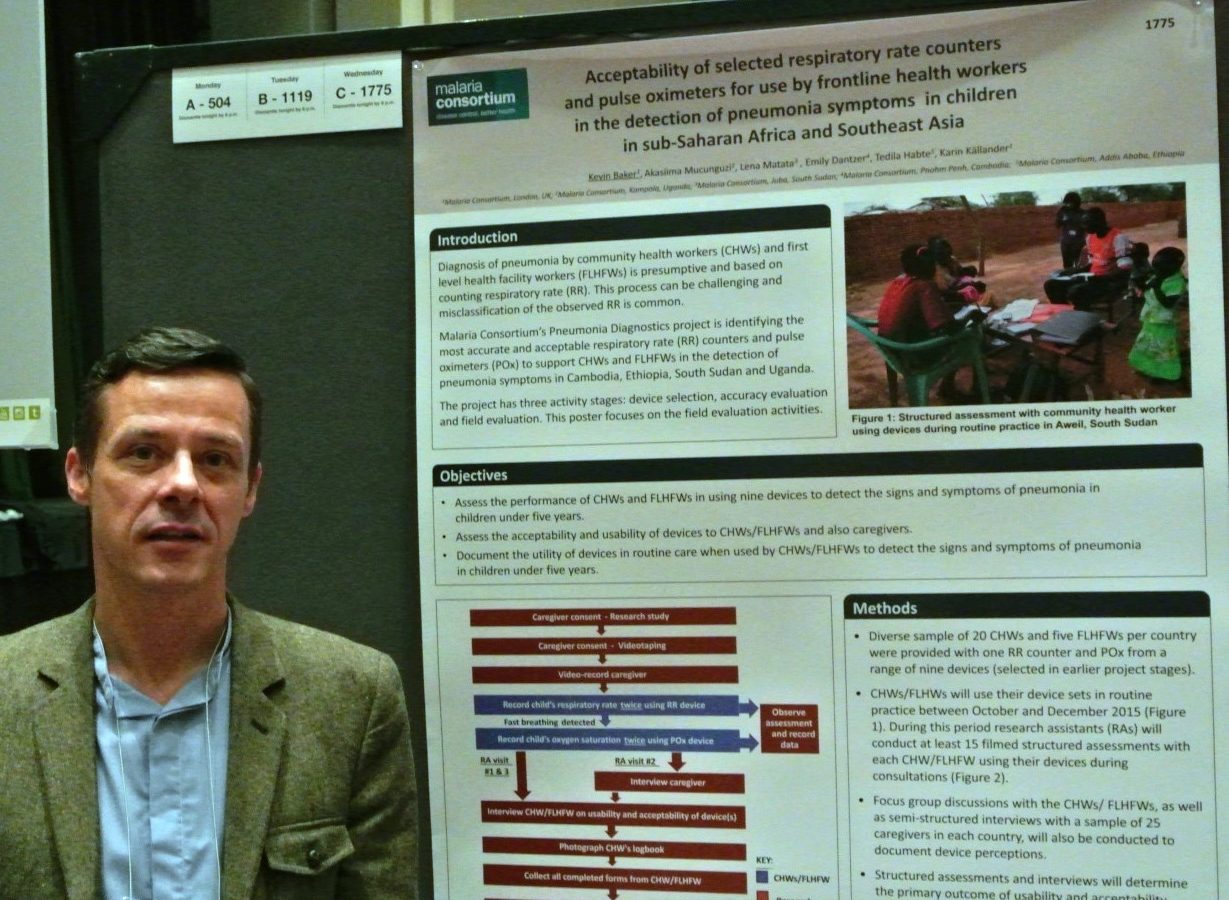
On Wednesday, the team presented two posters. The first went through our findings from the recently-completed ‘accuracy evaluation’ stage of the project, in which we assessed each tool in terms of how accurately it diagnosed pneumonia symptoms. This was the first time this data had been shared. The second poster gave an overview of the current ‘field evaluation’ activity, which evaluates the acceptability of the selected respiratory rate counters and pulse oximeters for frontline health workers.
On the evening of Wednesday October 28th, we held a side meeting at the conference to present on a number of topics.
We began the session by showing a film that outlined the current situation and specifically in Mulago Hospital in Uganda.
Dr Sylvia Meek, Malaria Consortium Technical Director, then gave a presentation that explained why pneumonia diagnostics was important to Malaria Consortium. She explained that because pneumonia remains the biggest infectious killer of children under five years, it is central to our mission to improve child health and builds on our work over the years in integrated community case management.
Dr Karin Kallander, Senior Research Advisor, went on to present on the role of respiratory rate timers and pulse oximeters in the detection of pneumonia in children in remote settings. Dr Kallander highlighted current activities and studies that are focused on developing and improving the management and treatment of pneumonia at the community level.
As Programme Coordinator, I gave the final presentation on data from the accuracy evaluation that was recently conducted for nine devices. This was the first time we presented this data for the five selected pulse oximeters. During the presentation, I proved that community health workers can use a range of pulse oximeters on children to accurately detect the signs of severe pneumonia (defined as oxygen saturation less than 90 percent). Three out of the five showed a mean difference of less than two percent, which was the agreed measure in this study. This means that these devices are considered to be accurate in the hands of community health workers when used to detect the signs of severe pneumonia. The results also showed that country differences are an important factor and need to be investigated further, in addition to further exploration of the different age strata in the study (0-60 days and 2-59 months), which performed differently (in general, devices were less accurate in the younger age strata).
We finished up with an interactive session where attendees had the opportunity to try out the devices for themselves. Participants found the devices easy to use and could see how they could be used at the community level. This was followed by a discussion on the need for robust devices which had reliable and long-life, rechargeable batteries.