Blog
Get insights and perspectives from our experts and the communities we work with about the impact of our activities
 7 March 2024
7 March 2024
International Women’s Day 2024: Seven ways to make health programmes gender intentional
To successfully reduce the gender equity gap in healthcare, we need to be gender intentional in our health programming. This means identifying and understanding gender inequalities, gender-based constraints, and inequitable norms …
 8 December 2023
8 December 2023
How can we leverage social and behaviour change to make malaria history?
As the team from Malaria Consortium interacted with over 130 delegates at the 2023 RBM Partnership to End Malaria Social and Behaviour Change Working Group meeting in Abidjan under the topic 'Amplifying Impact', the air buzzed wit…
 23 October 2023
23 October 2023
ASTMH Annual Meeting pinpoints research gaps to advance global health
In October 2023, Malaria Consortium participated in the 72nd Annual Meeting of the American Society of Tropical Medicine & Hygiene (ASMTH) in Chicago, USA. The conference brought together approximately 5,000 professionals from…
 19 October 2023
19 October 2023
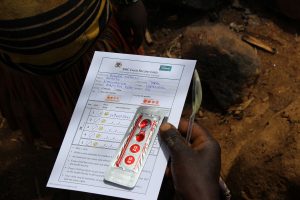
Showcasing our SMC research at the ASTMH Annual Meeting 2023
This year, Malaria Consortium proudly marks its 20th anniversary. Since its inception in 2003, our organisation has collaborated with governments and partners across Africa and Asia focusing on malaria and other targeted diseases.…
 7 September 2023
7 September 2023
Genetic interventions to combat obstinate mosquito-borne scourges
This piece was written for Outreach Network for Gene Drive Research and republished here, authored by Leo Braack, Co-Chair of APMEN Vector Control Working Group; Senior Vector Control Specialist from Malaria Consortium After ma…
Innovative health financing: How to make good on the promises of Africa’s new Public Health Order
Last month, a high level ministerial forum was convened by the African Centre for Disease Control (CDC) on the margins of the 36th Ordinary Session of the African Union Assembly. The meeting had notable Heads of State and Minister…
 3 November 2022
3 November 2022
ASTMH 2022: Transforming health through innovation
In the third and final instalment of our ASTMH blog series, we explore the need to prioritise innovation in public health programming to optimise the impact of interventions and help ensure more positive outcomes for the communiti…
 1 November 2022
1 November 2022
ASTMH 2022: The importance of equity and how we address it
In the second instalment of our ASTMH blog series, we outline some of Malaria Consortium's work around improving equitable access to health services and how this enables us to maximise the impact of our work. Yesterday in Seatt…
 31 October 2022
31 October 2022
ASTMH 2022: The power of partnerships to optimise health outcomes
In the first instalment of our American Society of Tropical Medicine & Hygiene's Annual Meeting (ASTMH) series this year, we're highlighting the powerful role of partnerships in delivering effective health interventions, stren…
 16 September 2022
16 September 2022
The impact of Global Fund investment in fighting malaria
The Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund) is a critical financing mechanism that has invested more than US$55 billion over the last 20 years to fund health programmes in countries with the highest burde…
 5 September 2022
5 September 2022
Eliminating malaria in the Greater Mekong Subregion
Around 15 years ago, worrying news from Asia made international headlines. There was evidence that new strains of the malaria parasite were developing resistance to artemisinin-derivatives. Used in combination therapies, these wer…
 19 August 2022
19 August 2022
The spectre of rising mosquito-borne urban disease
According to the United Nations, since 2007, more people globally are now living in cities than at any other time in history. In Africa, projections show that by 2030 the urban population will rise to 824 million – an increase o…
 20 July 2022
20 July 2022
Photo story: Eliminating malaria in Cambodia
Cambodia has achieved significant levels of malaria reduction but local, mobile and migrant populations in rural areas still lack access to malaria services. Through the Regional Artemisinin Initiative 3 Elimination (RAI3E), Ma…
 11 February 2022
11 February 2022
International Day of Women and Girls in Science 2022
Today marks International Day of Women and Girls in Science and the commitment the UN General Assembly made to achieve full and equal access to and participation in science for women and girls.
 13 January 2022
13 January 2022
Supporting country coordinating mechanisms to deliver Global Fund’s strategy
The Global Fund to Fight AIDS, Tuberculosis and Malaria recently released a new five-year strategy, following a long period of engagement with civil society and the global health community. The 2023–2028 strategy is entitled: Fi…
 15 November 2021
15 November 2021
COP26: What needs to happen next to secure the world’s health?
As COP26 draws to a close in Glasgow, it seems that we can be cautiously optimistic about the commitments that have been made. More than 100 countries have pledged to reverse deforestation by 2030; global banks, insurers and pensi…
 20 September 2021
20 September 2021
Malaria Consortium’s recommendations for the Global Fund 2023 strategy
The recently published Global Fund Results Report highlights the devastating impact the COVID-19 pandemic has had on the fight against HIV, TB and malaria in 2020. HIV and TB treatments and services have been hit particularly hard…
 13 September 2021
13 September 2021
Monoclonal antibodies: A breakthrough in the fight against malaria?
 10 August 2021
10 August 2021
Resilient health systems are vital in response to global warming
On 9 August, the Intergovernmental Panel on Climate Change (IPCC) released an eagerly anticipated landmark report on the impacts of global warming. The report highlights evidence asserting that changes to our climate have unequivo…
 23 March 2021
23 March 2021
Solar-charged solutions: Improving digital tools for community health workers in Mozambique
In 2016, we worked closely with the Ministry of Health in Mozambique and UNICEF to bridge the gap in community healthcare, developing the upSCALE mHealth app to assist community health workers, known locally as agentes polivale…
Load more